Medicare reimbursement for physicians is a mess.

I know, right?
One difficulty is getting reimbursed for all the stuff you have to do that’s not a face-to-face visit. Phone calls to check on medication compliance and coordinating with other providers is extremely important work. It pays dividends by saving money and improving outcomes over the long term. But until now, there’s been no way to get paid for that work.
That’s where the Chronic Care Management (CCM) Program comes in. It’s designed to help medical practices get paid for the valuable, but previously uncompensated, work required to care for patients with chronic illnesses.
Current procedural terminology (CPT) defines chronically ill patients as people diagnosed with two “chronic continuous or episodic health conditions that are expected to last at least 12 months, or until the death of the patient, and that place the patient at significant risk of death, acute exacerbation/decompensation, or functional decline.”
How to setup chronic care management
The Centers for Medicare & Medicaid Services (CMS) began reimbursing physicians for providing services outside the traditional face-to-face visit for fee-for-service Medicare patients with chronic diseases in January 2015. The CCM program covers previously unbillable services such as medication management or coordination with other specialists.
Services covered also include calling chronically ill Medicare patients to be sure they’re taking their meds, finding out why if they aren’t, and working to remedy the issue, as Dr. Jim King’s staff does at Prime Care Medical Center, his three-clinic practice in rural western Tennessee.
But not all doctors are signing up for reimbursement. CMS reported receiving reimbursement requests for only 100,000 of the 35 million Medicare beneficiaries eligible to receive qualified billable care-management services.
Multitudinous requirements, including extensive documentation, are keeping some doctors from taking advantage of the $42.60 per member per month they’re eligible for (that’s the 2015 average reimbursement adjusted based on geography).
Requirements:
Patients must have at least two eligible chronic conditions
Clinical staff must spend at least 20 minutes per month on services for them to qualify
Practices must create and maintain a comprehensive care plan
Practices must get written consent from the patient to implement the plan
Practices must use electronic health records (EHRs)
Practices must record data in a standardized format
Practices must ensure continuity of care
The calls from Dr. King’s office to check on medication compliance must add up to 20 minutes per month and be documented to qualify for reimbursement. And that doesn't include call prep time. This despite the fact that obviously the length of calls will vary widely month-to-month, ranging from 17 minutes per month to 70.
Some doctors are finding it tough to explain to patients why they’re facing a copay for services they used to get for free. Practices must collect 20% of the $42.60 from patients.
After that hurdle, patients must agree to allow the practice to be their CCM provider. Then the patient must understand and approve their comprehensive care plan. And comprehensive is the word.
Care plans must include:
Medication reconciliation and potential interactions
Medication adherence and patient self-management overview and review
List of all patient clinicians
Overview and periodic review of how the practice will coordinate with all patient clinicians
List of all patient health problems
List of all patient interventions
Patient prognosis
Measurable treatment goals
List of required social services
Overview and periodic review of how the practice will coordinate with social services
Assurance that care will take into account the patient’s choices and values
Strategies for managing symptoms and medication
Documentation requirements are no joke either. Check out this fairly comprehensive list of what you must document and how.
For doctors willing and able to play ball, the rewards can be significant.
Dr. King has been able to add one RN, two LPNs, and one clerk to his five-doctor, six-nurse staff. These new hires are in charge of leading the newly covered services; they make the follow-up calls, ensure the staff is following the patient-care plans, review test results, and work with the patients' other providers. Only a physician, advanced practice RN, clinical nurse specialist, or PA can bill CCM codes.
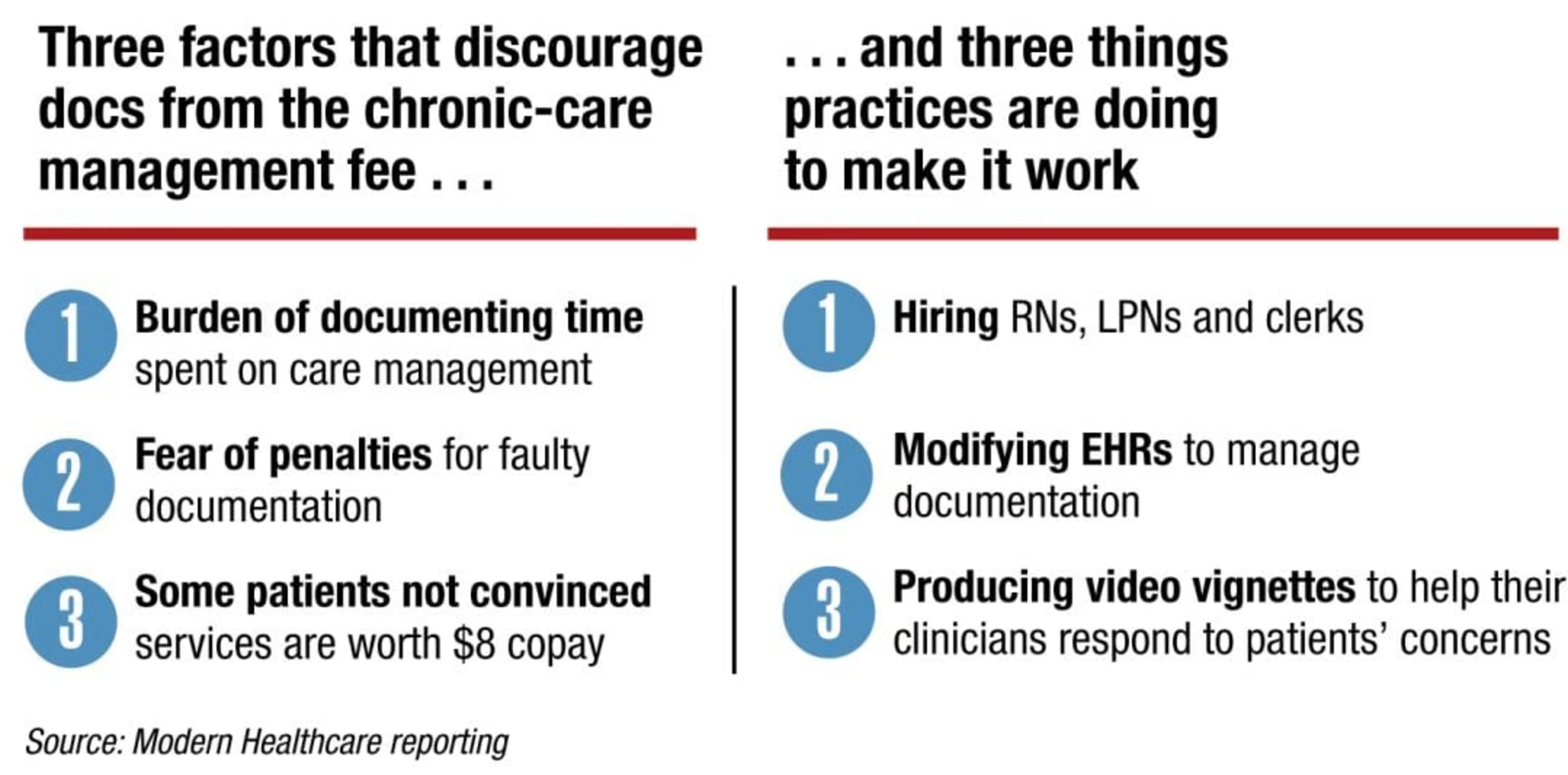
“At first sight, your thought is, 'For 40 bucks you want us to do all this?' Forget it,” Clinic Administrator Julie Sitzmann said. “Then you read closer, and it's stuff we're already doing—and documenting.”
EHR requirements
Medical Economics calls EHR limitations a “major reason” many practices will find it difficult to meet the CCM program requirements.
Despite the fact that Sitzmann’s municipally owned, Avera-managed, 25-bed facility is delivering qualifying services, they’re not billing the CCM (CPT code 99490). Family Medicine Clinics is a NCQA-recognized patient-centered medical home (PCMH). Experts say PCMHs are ideally suited to take advantage of this offer because many have already set up their workflows to improve care coordination.
But Family Medicine Clinics can’t take advantage of CCM program reimbursements because their EHR isn’t configured to record the required minute-by-minute documentation. According to the American College of Physicians, practices must use a certified EHR to use CPT code 99490. Practices are required to store their care plans in their EHRs to ensure all care team members have 24/7 access.
While some EHR systems include features that can support chronic care management, Medical Economics warns that most EHRs are not designed for facilitating collaboration among providers caring for the same patient. EHRs are limited in their ability to support care teams within practices because they try to replicate the paper records model.
Steven Waldren, MD, director of the AAFP’s Alliance for eHealth Innovation, criticises EHR vendors for building systems to fit an outdated, visit-oriented model of care. EHRs are built to allow a single physician to document everything that happens in a visit that can be used to justify billing, instead of to document everything a care team does.
This setup forces staffers to record what happens online and on the phone in the messaging section of the EHR. Later, the doctor goes in to move the information to where it belongs in the EHR.
“It’s mostly how you document it from a medico-legal standpoint, not how do you support and facilitate that type of collaboration [among care team members],” Waldren said.
They’re not designed to facilitate creating care plans as comprehensive as the ones CCM requires. They also generally lack the data analysis capabilities and automation required to deliver chronic disease care efficiently.
Practices looking to get reimbursed for after-hours care, such as for call coverage, must also ensure outside contracted clinicians, such as covering clinicians or locum tenens, have 24/7 access to the patient’s electronic care plan and electronic record and are under the general supervision of the CCM physician or “eligible practitioner.” This is another challenge for EHRs, as interoperability still lags despite the fact that practices must exchange care summaries in order to qualify for Meaningful Use.
Conclusion
The APC has a great outline of steps necessary to get started and a sample letter to patients. Stay tuned for EHR Requirements for the Chronic Care Management Program Part 2, where I will go into more detail on how you can make sure your EHR is ready for CCM.
In the meantime, let me know in the comments whether you’re planning to participate in CCM and why or why not.