Are medical staff satisfied with electronic health record systems? The answer changes from year to year and from study to study.
One 2014 survey indicated that 34% of physicians using EHRs were satisfied with their system – a fall from 62% in 2010. Physicians cited a negative impact on employee workflow, higher operating costs, and lower productivity than pre-launch as reasons for the decline.
But as unsatisfied as physicians might be, nurses are among the least satisfied with their EHR.
According to one survey by Black Book Market Research:
94% of nurses do not believe EHRs improve communication among staff.
90% believe their EHR has damaged their ability to communicate with patients.
Only 26% of nurses think that their system improves the quality of patient information.
As concerning as each of these numbers is on its own, each falls short of the 98% of nurses who say that they’ve never been included in their hospitals’ decisions in EHR implementation.
However, this last statistic is as much a reflection of poor EHR implementation as it is a cause.
Understanding why nurses dislike EHRs
Nurses have a variety of reasons for disliking their system, and these reasons often stem from misunderstandings about how EHRs work. Dissatisfied nurses will frequently cite lower productivity or communication troubles; but these issues can be considered symptoms of being ignored during the planning stage.
“Nurse productivity problems can be sourced to the failure of those selecting and implementing an EHR to involve direct care nurses in the process,” according to Doug Brown of BBMR. Nurses’ problems can be traced back to the fact that they are rarely considered key stakeholders in planning, despite being some of the most routine users of EHRs.
Without collaboration before launch, medical staff are more likely to access and record patient information differently, resulting in confusion, repeat entry, and miscommunication with patients.
For example, new nurses entering the field may be more familiar with EHRs as they are a commonplace subject in nursing curriculum today, but veteran nurses may not be as familiar with the technology, resulting in clashes in how staff members coordinate.
Overcoming barriers of use

Nurses are often taught to rely heavily on workarounds and templates rather than fully comprehending the EHR. This lack of proper training results in problems with usability when shortcuts aren’t possible.
Another common scenario that indicated a healthcare organization has failed to adequately include nurses in EHR planning is when opinion on the quality of a system depends on personal computer literacy instead of the merits of the system. For example, nurses with experience in computer use had an 80% more favorable attitude towards EHRs than those without experience, at a major hospital in Southwest Florida.
When an organization fails to help employees overcome basic barriers to use such as computer literacy, this can be a red flag that management failed to assess employees’ needs and provide ample training – which all need to be part of an EHR’s launch.
Implementing Electronic Health Records

Before they can address nurses’ concerns administrators need to know the steps for successful EHR implementation and the role that nurses need to play in each step.
The Health Resources and Services Administration has established nine recommended steps that can guide the use of new EHRs, illustrated in the infographic below.
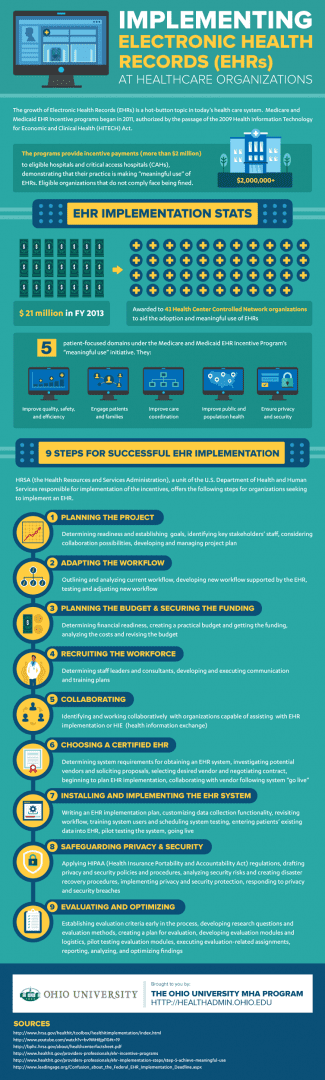
Source: The Ohio University MHA Program
Several of these steps pertain to nurses throughout pre-launch:
Planning the project: By establishing productivity goals for each member of staff towards achieving meaningful use and considering collaboration possibilities between staff in advance, managers are better able to recognize and overcome barriers to use. A project plan also enables better communication on the value of the new system for greater buy-in.
Adapting the workflow: One of the most intimidating aspects for nurses beginning to use EHRs is uncertainty of how it will impact their workflow. Nurses need an opportunity to become familiar with the system so that it becomes integrated in their process – not a disruption to it.
With ample training to learn how they can participate in the entry of information, nurses can discover new ways save time for themselves and other medical staff.
Installing and implementing the EHR system: Nurses should know how to record all of their activities accurately in an EHR well before launch day. Simulations can be effective in illustrating of how data should be accessed and logged in different situations, such as finding a patient’s exam room or logging phone calls.
Recruiting the workforce: According to Black Book’s survey, nearly seven out of ten nurses consider their hospital’s IT department incompetent. Administrators are less likely to comprehend the level of IT support needed for the project without the input of nurses.
By identifying nurses’ technical skillsets beforehand, managers can more effectively gauge the need for additional support staff. Hospitals can also hire temporary nursing and technical staff during initial training to ease the workload on nurses learning new skills.
Safeguarding privacy and security: Another key reason EHRs have generated controversy is due to the questions of how they impact patient privacy, and whether these systems are capable of maintaining that privacy. Nurses must be involved in the planning stage for briefing on best practices to ensure that patient information remains secure.
Evaluating and optimizing: Your planning needs to include a means of evaluation to get an idea of how the EHR is impacting your productivity. Introducing nurses to these criteria before launch will better establish expectations while encouraging a productivity-minded approach across your team.
Conclusion:
One of the greatest frustrations of nurses’ low approval of EHRs is that these individuals can bring unique, valuable perspectives to the table during implementation. Having their voices heard during implementation can help nurses more readily accept a new system, while introducing new ideas about ways the technology can enhance collaboration and communication across staff and patients alike.
If your healthcare organization is getting ready to implement a new EHR, including your nurses in the pre-launch process is an invaluable measure to help your staff understand how the system can benefit your team – and maybe even learn to love EHRs in the process.