Cerner's name is derived from a Latin word meaning "to discern."
Epic takes its name from the long poems usually written down from oral tradition; the Greek poet Homer wrote the most famous of them.
The Romans might have defeated the Greeks in the Battle of Corinth, but in the battle between these two EHRs with ties to the ancient civilizations, no clear winner has been declared.
The most recent Kalorama Information Report names Cerner and Epic as two of the top three EHR vendors along with McKesson.
Cerner is the more widely used option, coming in at No. 7 on our Top 20 Most Popular EHR Software options list, with Epic not far behind, at No. 11.
Epic is gaining steam, though, with efforts to appeal to smaller hospitals and physician practices underway. For example, in February, Epic CEO Judy Faulkner told HealthcareITNews that Epic will come in three versions as opposed to just one, though she didn't give a timeframe.
One of the new offerings, Epic Sonnet (as in a poem shorter than an epic), will be a lighter version of Epic. It's missing a few features, but it's offered at a lower price. Epic is also hiring pros to help them start a new medical billing unit.
For its part, Cerner recently introduced Cerner RevWorks, a solution meant to improve revenue cycle management.
Epic's efforts to woo the smaller provider market seem to be working. KLAS researchers recently announced that Epic controls 25.8% of the market for acute-care hospitals, which tend to be smaller. Cerner is second, with 24.6% of the market. Epic has been the leading vendor for six years running, in part because no small hospitals have reported voluntary uninstalls, as of yet.
Here's how these two healthcare giants compare side-by-side. We're looking at:
Installation and implementation
Integrations and interoperability
User interface (UI)
Customer support
Installation and implementation
“EHR implementations are notorious budget-busters often fraught with missed deadlines and other unforeseen complications," writes Tom Sullivan for HeathcareITNews.
So it's important to consider the time, cost, and effort involved in implementing a new EHR. Unfortunately, neither Cerner nor Epic has a great record for smooth, successful, timely, or under-budget implementations.
In one example, Vancouver Island Health Authority in Canada went back to using paper order forms after claiming that their March 2016 Cerner implementation "lost, buried, and changed orders for drugs and diagnostic tests" at random.
So far, Cerner has not announced that it has any big changes in the pipeline regarding installation or implementation.
A similar fate befell Epic, with the U.S. Coast Guard. A deal to serve 178 sites fell through after five years of attempted implementation.
“Epic EHR installations are known to cost millions of dollars," writes Bernie Monegain for HealthcareITNews.
“More often than not, it seems that Epic rollouts end up costing a great deal more than expected," writes veteran healthcare consultant and analyst Anne Zieger. New York City's Health and Hospital Corp. agreed to a $302 million Epic implementation in 2013. As of 2016, they'd paid $764 million, with overall costs of up to $1.4 billion. “If I were still on the fence I'd find numbers like those more than a little concerning," Zieger writes. “And they're far from unique."
One major expenditure involved in installing Epic is the need to hire IT staff. However, at last year's Users Group Meeting, Faulkner announced that Epic employees will start completing more installations for hospitals. Epic employees should be able to accomplish installation faster and with fewer errors. This move will also save hospitals money they'd otherwise have to spend hiring more IT technicians.
Integrations and interoperability
Your EHR won't be effective if people in your organization refuse to fully embrace it. HealthcareITNews polled 95 healthcare executives in October 2016 about their healthcare tech needs, and 60% of respondents say they'll work on integrating their EHRs with other technologies in 2017 to entice more physicians and nurses to use them.
Healthcare organizations plan to focus on interoperability projects such as:
Connecting to external databases, such as health information exchanges (65%)
Connecting applications within the organization (58%)
Adding connections from medical devices to existing systems (37%)
Both Cerner and Epic are part of the privately-funded Argonaut Project, along with some competing EHRs and Beth Israel Deaconess Medical Center and Mayo Clinic. The goal is to promote adoption of the Fast Healthcare Interoperability Resources (FHIR), a set of specifications and an application programming interface (API).
As part of its commitment to integration, Cerner has built three platforms that integrate with each other and with external systems to connect clinical, operational, and financial data.
In an interview at health IT conference, HIMSS17, Cerner President Zane Burke indicated the vendor is making efforts to create application program interfaces (APIs) which will increase interoperability not just with other EHRs, but with third-party software and apps for mHealth, population health, and information exchange.
In addition, interoperability is one of Cerner's core initiatives. The company is a founding member of the CommonWell Health Alliance, a nonprofit and independent organization focused on developing and deploying interoperability solutions.
Its website also offers the Interoperability Ticker, an interactive map that tracks clinical transactions, pharmacy transactions, health information exchanges, and Cerner interoperability solutions in use across the country.
Epic has been criticized for offering no integrations and less interoperability than its competitors. For example, Epic has refrained from joining certain marketplace collaborations that claim to be dedicated to interoperability, such as the CommonWell Health Alliance.
But over the past two years Epic has made great strides. The vendor is a founding member of the Carequality Interoperability Framework, which facilitates health data exchange between more than 3,000 clinics and 200 hospitals, public and private, using a variety of EHRs.
In addition, interoperability concerns didn't dissuade Mayo Clinic CIO Cris Ross from making the switch from Cerner to Epic. “When we looked at [Epic's] ability to connect via the Direct protocol to many other EHRs, and the volume that's floating across that network, from Epic to other EHRs, we were pretty impressed," Ross tells Healthcare IT News. “The fact that they have such robust connectivity to other EHRs as well really alleviated that concern for us."
User interface (UI)
Seeking an improved UI is also among the strategies healthcare executives plan to turn to for increased EHR use, with 47% putting it first on their list.
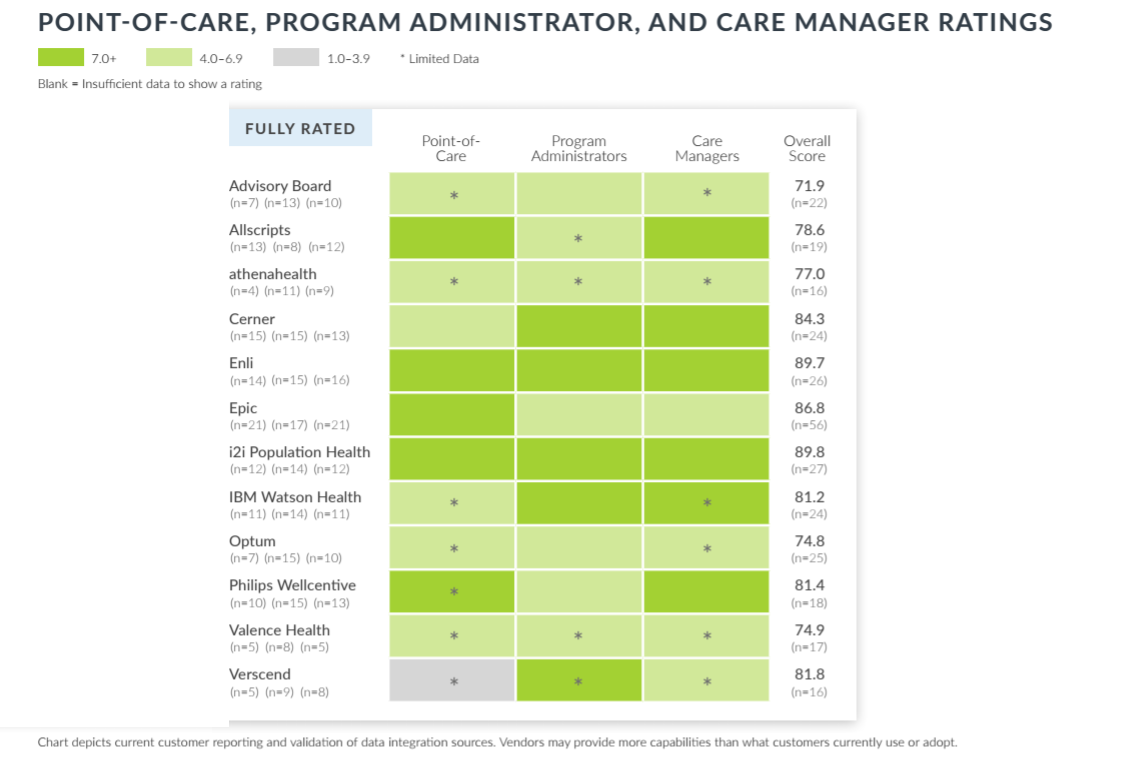
A new report from KLAS has Cerner ranked fourth, just below athenahealth, in usability, according to care managers, program administrators, and clinicians at the point of care.
But Software Advice reviewers have complained that Cerner's UI is “not as intuitive as I would like." Another reviewer writes, “Without [the vendor] standing behind the doctors and nurses, charting on this system would be impossible. This system could actually push physicians to early retirement."
It is, in another reviewer's estimation, “extremely difficult to navigate," and “takes away from patient care." They go on, “I've used an EMR in my office for 14 years, and this new system is unbelievably cumbersome and nonintuitive."
“The software is poorly designed, difficult to navigate, and generally feels like it was designed by engineers who have never worked in a healthcare setting," another user writes.
According to EHRsoftware.us, many Epic customers have praised that software for being “quick to implement and easy to use."
However, Software Advice reviewers are more critical of Epic's UI. Many complain about the time it takes to learn the system. “It is hard to learn because it is so complex," is one comment that represents a perspective shared by many. Another says there are “too many contexts to switch between."
Others, though, are more impressed. “I find this the best EMR system," one user writes. “It is very easy to navigate between documents and write orders and notes. A lot of valuable presets and [the] ability to create templates. As a med student I used a lot of different systems and this is my favorite!" Another writes that Epic is “way [easy] to use in terms of navigation."
The overall takeaway from the reviews appears to be that, once you've learned to use Epic, it's fairly streamlined.
Customer support
Cerner offers 24/7 live support. One Software Advice reviewer glows that Cerner offers a “great support team." Another writes, “The support staff has been very helpful."
One Capterra reviewer says that Epic “gives excellent technical support." But otherwise no comments.
Who will have hegemony?
Greece ultimately fell to Rome, but who will win the battle between these EHRs is still unknown.
Cerner is the better option for health delivery organizations that need access to support 24/7, great interoperability and many integrations, and better population health management functionality, at least for now.
Epic is the right choice for a pleasing UI, help with installation, and billing help, all of which are very useful for smaller organizations with smaller staffs.
To compare more options, check out our EHR directory.
Or to read more about how Cerner and Epic compare to other EHRs, check out these articles: